Many people associate mouth cancer almost exclusively with smoking or tobacco use. So when someone who has never smoked is diagnosed, it often feels confusing and unexpected. This gap between perception and reality is why so many people go online searching for answers.
The truth is that mouth cancer among nonsmokers is a recognised medical condition, and its incidence has been gradually increasing. Factors beyond tobacco, such as viral infections, long-standing oral irritation, immune health, and genetic susceptibility, can quietly affect the cells of the mouth over time. Understanding these influences helps explain why non-smokers can also develop oral cancer.
This article is written to address the questions people commonly search for when they are trying to make sense of this diagnosis. It explains why non-smokers get mouth cancer and outlines the leading causes of oral cancer in non-smokers in a clear, relatable, and reassuring way, with the aim of supporting early awareness and informed decision-making.
Can You Get Mouth Cancer If You Never Smoked?
Yes. You can develop mouth cancer even if you have never smoked, chewed tobacco, or consumed alcohol. While tobacco remains a major risk factor, a significant number of oral cancer cases occur in non-smokers due to other medical, viral, and environmental causes.
This is why we at our clinic increasingly see mouth cancer in non-smokers, including younger adults and people with otherwise healthy lifestyles.
Why Do Non-Smokers Get Mouth Cancer?
People often search why non-smokers get mouth cancer because the condition feels unexpected. The answer lies in factors that can damage oral cells over time, even without tobacco exposure.
Common reasons include viral infections like HPV, long-standing oral irritation, weakened immunity, genetic susceptibility, and nutritional deficiencies. These factors can silently affect the mouth lining and lead to abnormal cell growth.
Why Non-Smokers Can Get Mouth Cancer? (14 Reasons)
Mouth cancer can develop even without smoking because cancer is ultimately caused by damage to oral cells and failure of normal repair mechanisms, not tobacco alone. In non-smokers, this damage comes from several well-recognised pathways.
1. Human Papillomavirus (HPV) Infection
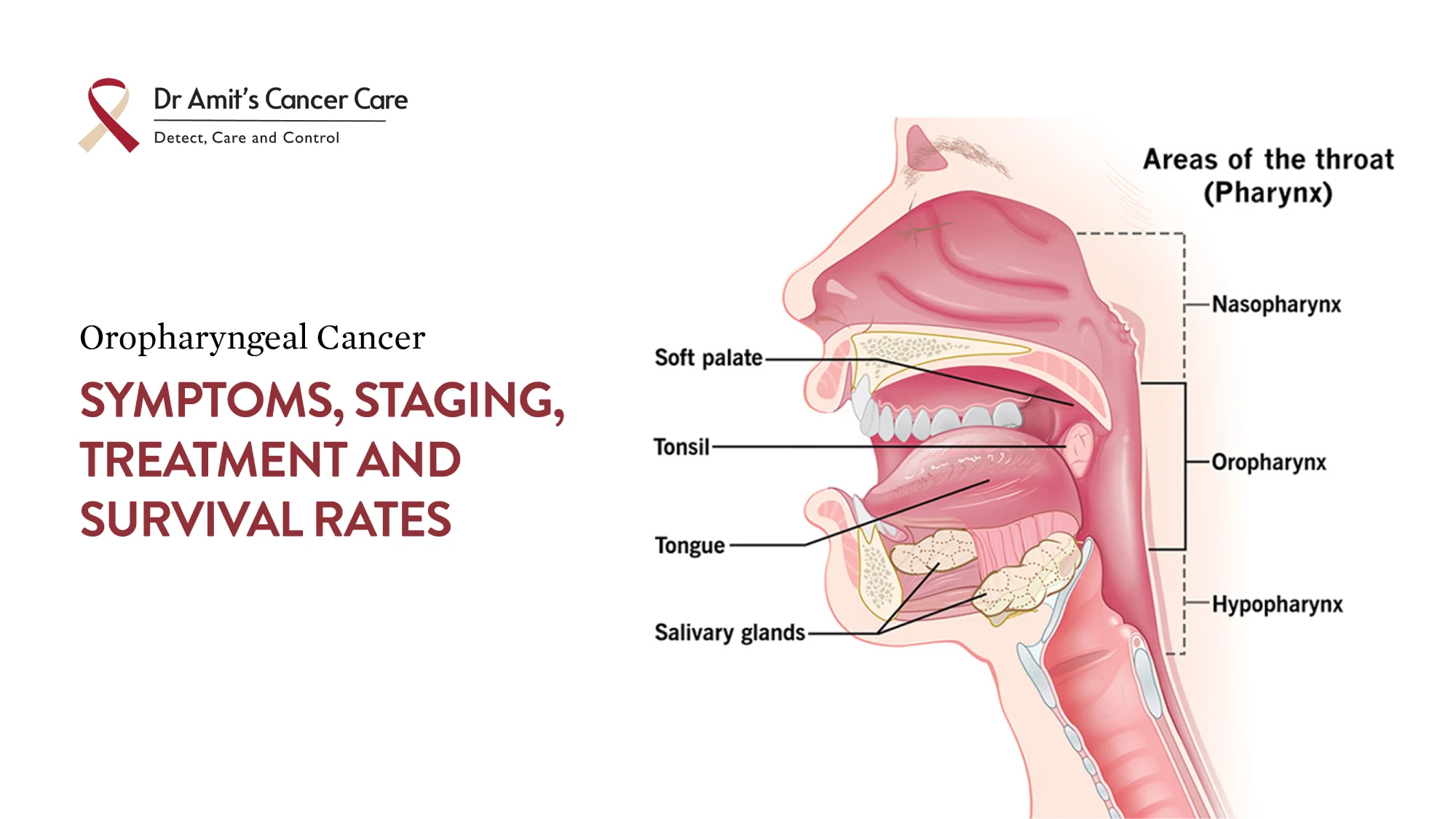
HPV, particularly HPV-16, is one of the most important causes of oral and tongue cancers in non-smokers. The virus integrates into oral cell DNA and triggers abnormal cell growth over time. HPV-related cancers are increasingly common, especially in younger adults.
2. Chronic Oral Irritation or Trauma
Long-term irritation inside the mouth can increase cancer risk. This includes sharp or broken teeth, poorly fitting dentures, rough dental restorations, habitual cheek or tongue biting, and non-healing ulcers. Continuous injury promotes inflammation and abnormal cell repair.
3. Alcohol Consumption Without Smoking
Alcohol alone can damage the lining of the mouth, increase inflammation, and reduce the protective barrier of oral tissues. Regular or heavy alcohol use is a known independent risk factor, even in lifelong non-smokers.
4. Poor Oral Hygiene and Gum Disease
Chronic gum disease, untreated dental infections, and long-standing inflammation create an unhealthy oral environment. This persistent inflammation can contribute to DNA damage and cancer development over time.
5. Nutritional Deficiencies
Nutrition plays a key role. Deficiencies in vitamins and minerals essential for cell repair increase risk. Low levels of vitamin A, vitamin C, vitamin E, iron, and folate reduce the body’s ability to protect and regenerate oral tissues.
6. Weakened or Suppressed Immune System
A weakened immune system may not eliminate abnormal cells effectively. Causes include chronic medical conditions, long-term medications, severe stress, malnutrition, or immune-suppressing illnesses.
7. Genetic Susceptibility
Some individuals inherit genetic traits that affect DNA repair or immune surveillance. This means cancer-causing mutations can still happen, even in the absence of tobacco or alcohol.
8. Family History of Oral or Head-and-Neck Cancer
A family history of mouth, tongue, or throat cancer may increase risk due to shared genetic or environmental factors, even among non-smokers.
9. Precancerous Oral Conditions
Conditions such as leukoplakia (white patches in the mouth that do not rub off), erythroplakia (persistent red patches with a higher risk of malignant change), and oral submucous fibrosis (chronic stiffening of oral tissues that restricts mouth opening) can progress to cancer if not monitored or treated. These conditions may occur even without smoking.
10. Excessive Sun Exposure (Lip Cancer)
Prolonged ultraviolet exposure is a major cause of lip cancer, particularly of the lower lip. This is common in outdoor workers and individuals without sun protection.
11. Occupational and Environmental Exposures
Exposure to certain chemicals, dusts, fumes, or pollutants in industrial or environmental settings can contribute to oral cancer risk over time.
12. Chronic Viral or Fungal Infections
Long-standing infections in the oral cavity can cause repeated inflammation and cellular stress, increasing susceptibility to malignant change.
13. Age-Related Cellular Changes
As people age, natural DNA repair mechanisms become less efficient. This increases cancer risk even without traditional lifestyle risk factors.
14. Poorly Controlled Diabetes and Metabolic Disorders
Chronic metabolic conditions can impair immune response, wound healing, and cellular regulation, indirectly increasing cancer risk.
Mouth cancer does not develop from a single cause. In non-smokers, it usually results from a combination of factors acting over time. This is why people with healthy lifestyles can still develop oral cancer.
Is Mouth Cancer Common in Non-Smokers?
Mouth cancer is still more common in tobacco users, but cases in non-smokers are steadily increasing. Doctors are now seeing more patients with mouth cancer in non-smokers, especially HPV-related cancers of the tongue and throat.
This trend is one of the main reasons awareness campaigns now emphasise that oral cancer is not limited to smokers.
Can Poor Oral Hygiene Cause Mouth Cancer?
Poor oral hygiene alone does not directly cause cancer, but it can contribute indirectly. Chronic infections, gum disease, and long-standing inflammation create an unhealthy environment in the mouth. Over time, this may increase susceptibility to cancer, particularly in non-smokers with other risk factors.
Can Stress or Diet Cause Mouth Cancer?
Stress itself does not cause mouth cancer, but long-term stress can weaken immunity and affect healing. Diet plays a more direct role. Diets low in fruits, vegetables, and antioxidants may reduce the body’s ability to repair damaged cells.
Nutritional deficiencies are recognised as contributing to the causes of oral cancer in non-smokers.
Can Mouth Cancer Go Away on Its Own?
No. Mouth cancer does not cure itself. If left untreated, it usually progresses. Some early lesions may appear harmless, which is why people delay evaluation. Early diagnosis is critical, especially for non-smokers who may not suspect cancer.
What Are the Early Signs of Mouth Cancer in Non-Smokers?
People often search for symptoms because they assume cancer is unlikely without smoking. Warning signs include:
- A mouth ulcer that does not heal within two weeks
- White or red patches inside the mouth
- Persistent pain or numbness
- Difficulty chewing or swallowing
- A lump in the neck or jaw
These symptoms should be evaluated promptly, regardless of smoking history.
Is Mouth Cancer Curable in Non-Smokers?
Yes. Mouth cancer in non-smokers is often highly treatable, especially when detected early. In fact, some HPV-related oral cancers respond well to treatment and have favourable outcomes.
Early-stage detection remains the strongest factor influencing cure rates.
Should Non-Smokers Get Regular Oral Cancer Checks?
Yes. Regular dental and medical check-ups are important for everyone, including non-smokers. Dentists and doctors can identify suspicious changes early, often before symptoms become severe.
This proactive approach significantly improves outcomes for mouth cancer in non-smokers.
Key Takeaway
Mouth cancer is not limited to smokers. Mouth cancer in non-smokers can occur due to HPV infection, chronic irritation, alcohol use, immune-related factors, genetic susceptibility, and nutritional issues. Understanding why non-smokers get mouth cancer helps break long-standing myths and encourages earlier evaluation of symptoms that might otherwise be ignored.
If you notice persistent changes in your mouth, seeking timely medical advice can make a meaningful difference. An evaluation by an experienced oncosurgeon such as Dr Amit Chakraborty can help clarify concerns early and guide the next steps with confidence. Early awareness saves lives, regardless of smoking history.