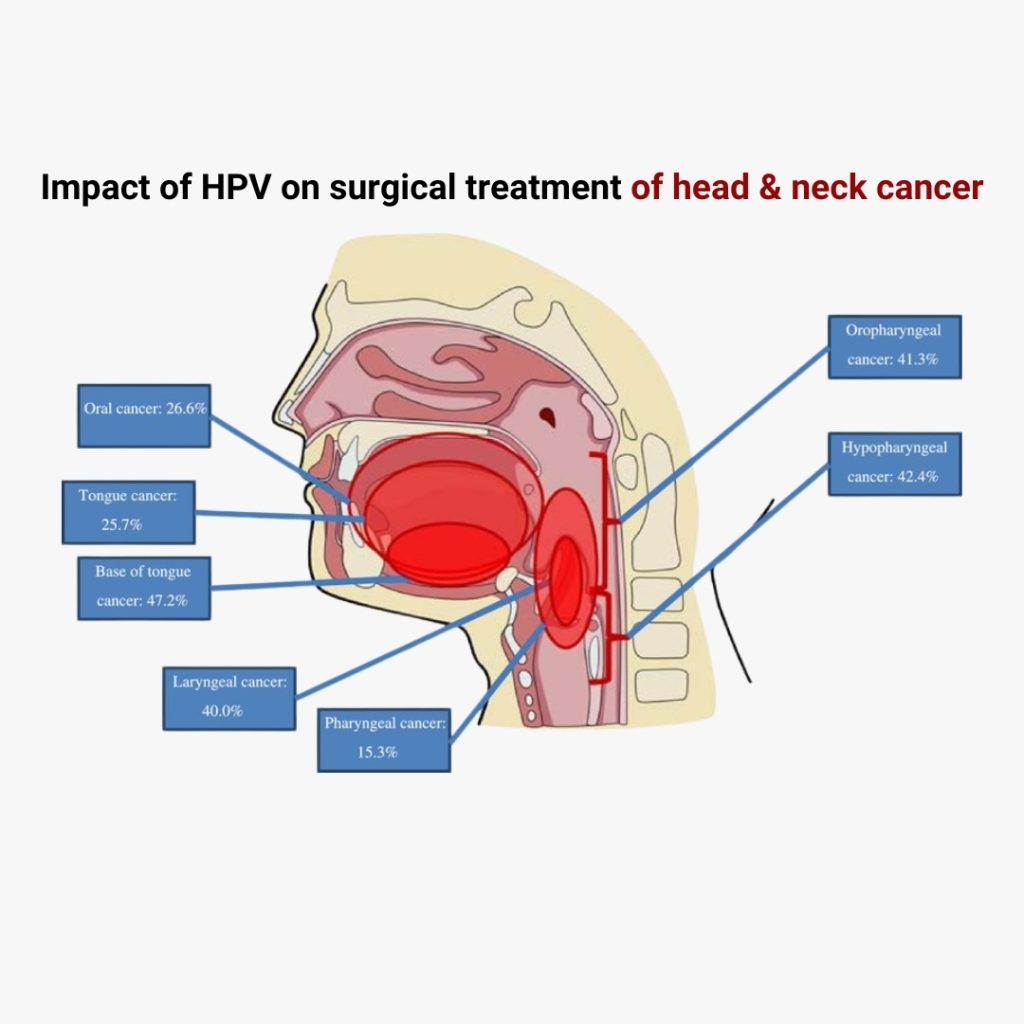
Head and neck cancers are among the most challenging forms of cancer to treat due to their proximity to vital structures in the body, such as the mouth, throat, and voice box. One key factor that has changed the landscape of treating these cancers in recent years is the increasing link between human papillomavirus (HPV) and head and neck cancer, especially oropharyngeal cancer.
HPV-positive head and neck cancers tend to behave differently from those caused by traditional risk factors like smoking and alcohol. This has a significant impact on the way cancer specialists and surgical oncologists approach treatment, particularly when surgery is considered.
Understanding HPV-Positive Head and Neck Cancers
HPV is a common virus that can cause infections in various parts of the body, and it is now recognized as a major risk factor for certain types of head and neck cancers, particularly those affecting the oropharynx (the middle part of the throat, including the tonsils and the base of the tongue). Unlike cancers caused by tobacco or alcohol, HPV-positive cancers often occur in younger, healthier patients who don’t have a history of smoking or drinking.
The behavior of HPV-positive cancers is different in several ways:
– They tend to respond better to treatment.
– Patients with HPV-positive head and neck cancers generally have better outcomes and longer survival rates.
– They may require less aggressive treatments than their HPV-negative counterparts.
These differences have led to a shift in the way surgical oncologists and other cancer treatment specialists manage these cases.
The Role of Surgery in Treating HPV-Positive Head and Neck Cancers
When it comes to treating HPV-positive head and neck cancers, surgery remains a critical option. However, advances in the understanding of HPV have allowed oncologists to tailor surgical approaches that are more effective and less invasive.
Minimally Invasive Surgical Techniques
Thanks to the typically better prognosis for HPV-positive cancers, many surgical oncologists in Mumbai and around the world now focus on minimally invasive surgical techniques. These techniques, such as transoral robotic surgery (TORS) and laser microsurgery, allow cancer specialists to remove tumors with greater precision, resulting in:
– Reduced damage to surrounding healthy tissue.
– Faster recovery times.
– Better preservation of important functions like speech and swallowing.
Patients undergoing these minimally invasive surgeries often experience fewer side effects and can maintain a higher quality of life compared to those treated with more extensive surgeries.
Balancing Surgery with Other Treatments
One of the key challenges for cancer treatment specialists is determining the balance between surgery, radiation therapy, and chemotherapy. While surgery can be highly effective for removing HPV-positive tumors, many patients may also benefit from additional treatments to ensure all cancer cells are eradicated.
However, because HPV-positive cancers tend to be more responsive to radiation and chemotherapy, oncologists may opt for less aggressive surgery followed by these treatments. In some cases, surgery may be avoided altogether if radiation or chemotherapy alone can effectively treat the cancer.
HPV’s Impact on Treatment Outcomes
The presence of HPV in head and neck cancers has significantly improved patient outcomes. Studies show that patients with HPV-positive oropharyngeal cancers have a higher survival rate and are more likely to respond favorably to treatments compared to HPV-negative patients.
For a surgical oncologist in Mumbai, the presence of HPV can be a critical factor in determining the course of treatment. The improved prognosis allows oncologists to reduce the intensity of treatments, sparing patients from the often debilitating side effects of traditional therapies. This approach leads to better overall outcomes and a higher quality of life post-treatment.
HPV Vaccination and Prevention
One of the most effective ways to reduce the incidence of HPV-related head and neck cancers is through vaccination. The HPV vaccine, commonly recommended for adolescents, has been shown to prevent infections that can lead to these cancers later in life.
As awareness of the link between HPV and cancer grows, cancer specialists are advocating for widespread vaccination as a preventive measure. In the long term, this could drastically reduce the number of patients requiring surgical intervention for HPV-related head and neck cancers.
Consulting a Surgical Oncologist in Mumbai
If you or a loved one has been diagnosed with HPV-positive head and neck cancer, it is crucial to consult with an experienced surgical oncologist in Mumbai. They will work alongside a team of cancer treatment specialists to develop a personalized treatment plan that takes into account the unique nature of HPV-positive cancers. With the right approach, patients can expect excellent outcomes and a higher chance of recovery.
Conclusion
HPV has revolutionized the way head and neck cancers are treated, especially in terms of surgery. With a better understanding of the virus and its effects on cancer progression, oncologists are able to offer more tailored and less invasive treatments, improving patient outcomes. As research continues and awareness of HPV grows, the future of head and neck cancer treatment looks increasingly hopeful.