Surgical Management of Hypopharyngeal Cancer: A Comprehensive Guide
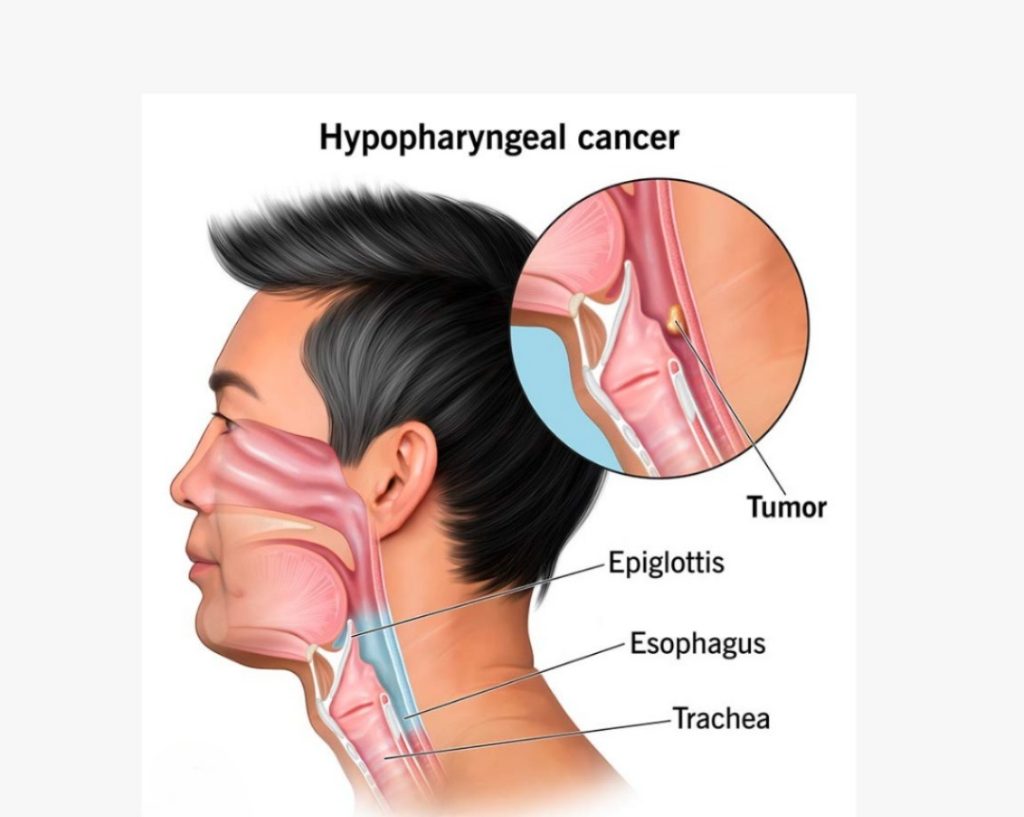
Hypopharyngeal cancer is a relatively rare but aggressive form of head and neck cancer, originating in the hypopharynx, which is the part of the throat located behind the larynx and above the esophagus. Effective management of hypopharyngeal cancer requires a multidisciplinary approach, with surgery playing a crucial role, especially in locally advanced cases. This guide outlines the key aspects of surgical management for hypopharyngeal cancer.
Overview and Indications for Surgery
Surgery is often indicated for hypopharyngeal cancers that are resectable and in patients who are suitable surgical candidates. It is typically considered in the following scenarios:
–Early-stage disease (Stage I and II): Surgery can be curative and often involves less extensive procedures, sometimes followed by radiation therapy. Consulting with a surgical oncologist in Mumbai can provide expertise in these early stages.
–Locally advanced disease (Stage III and IV): Surgery is often combined with radiation therapy and/or chemotherapy. The goal of surgical intervention is to remove the tumor completely, leaving visible margins. For advanced cases, finding the best oncology specialist in Mumbai is crucial for comprehensive care.
–Recurrence: Surgical salvage can be considered for recurrent disease after initial radiation or chemoradiation.
Preoperative Assessment and Planning
A thorough preoperative evaluation is crucial for optimizing surgical outcomes and minimizing complications. Key aspects include:
-Staging: Accurate staging using imaging modalities like CT, MRI, and PET scans is essential to assess the extent of the primary tumor, regional lymph node involvement, and distant metastases. For the most precise staging, consult the best oncology center in Mumbai.
–Nutritional Status: Many patients with hypopharyngeal cancer are malnourished due to dysphagia. Nutritional support, including gastrostomy if needed, should be optimized preoperatively.
-Airway Management: Due to the tumor's location, airway management must be carefully planned. Tracheostomy may be required before surgery to secure the airway.
–Multidisciplinary Team Discussion: Input from surgeons, oncologists, radiologists, nutritionists, and speech therapists is vital for comprehensive planning.
Engage with the top surgical oncologists in Mumbai for a well-coordinated approach.
Surgical Techniques
The choice of surgical approach depends on the tumor's location, size, extent, and involvement of adjacent structures. The main surgical options include:
-Partial Pharyngectomy: This procedure involves the resection of part of the hypopharynx. It's indicated in small, localized tumors and aims to preserve as much of the hypopharyngeal function as possible.
-Total Laryngopharyngectomy: In this procedure, the hypopharynx, larynx, and occasionally a section of the esophagus are removed. It is typically performed for extensive tumors or when partial resection is not feasible. A tracheostomy is performed to maintain an airway, and reconstructive techniques are employed to restore swallowing function.
–Neck Dissection: Given the high propensity for regional lymph node metastasis, neck dissection is often performed in conjunction with the primary tumor resection to manage regional lymphatics.
-Reconstructive Surgery: Reconstruction is a crucial component of surgical management to restore function and appearance. Options include:
-Primary Closure: Used for small defects.
-Regional Flaps: Like the myocutaneous pectoralis major flap.
-Free Flaps: Such as radial forearm free flaps or jejunal free flaps, used for extensive defects requiring more complex reconstruction to restore swallowing and speech function.
Postoperative Care and Complications
Postoperative care focuses on monitoring for complications, ensuring adequate nutrition, and managing the airway. Key aspects include:
-Airway Management: A temporary or permanent tracheostomy is frequently necessary for patients. Suctioning and proper maintenance are necessary to avoid issues.
-Nutritional Support: Enteral feeding is continued until the integrity and function of the reconstructed hypopharynx are confirmed.
-Speech and Swallowing Rehabilitation: Early involvement of speech therapists is crucial to help patients adapt to the changes in anatomy and function, especially following extensive resections.
-Wound Care and Infection Prevention: Meticulous care of the surgical site is necessary to prevent wound complications, which are common due to the proximity of the upper aerodigestive tract.
Complications
Following surgery for hypopharyngeal carcinoma, the following side effects are possible:
–Fistula Formation: Pharyngocutaneous fistulas are a common complication, particularly after laryngopharyngectomy.
–Bleeding and Hematoma: Careful intraoperative hemostasis and postoperative monitoring are required.
–Infection: Patients are at risk of wound infections and systemic infections due to compromised nutritional and immune status.
– Dysphagia and Aspiration: These functional complications are common, and their management requires a multidisciplinary approach involving dietitians, speech therapists, and, in some cases, further surgical intervention.
Outcomes and Prognosis
Surgical management offers the potential for cure, particularly in early-stage disease. However, the prognosis of hypopharyngeal cancer is often poor, with 5-year survival rates ranging from 20% to 60%, depending on the stage at diagnosis. Locally advanced and recurrent diseases carry a worse prognosis.
Functional outcomes, including voice and swallowing, vary significantly depending on the extent of surgery and the success of reconstruction. Quality of life considerations, including the potential need for permanent tracheostomy or gastrostomy, play a vital role in surgical decision-making.
Conclusion
Surgical management of hypopharyngeal cancer is complex and requires careful planning, a multidisciplinary approach, and individualized patient care. Advances in surgical techniques and reconstructive options continue to improve outcomes and quality of life for patients with this challenging disease. Postoperative care, rehabilitation, and ongoing surveillance are critical components of comprehensive cancer care, aimed at optimizing functional outcomes and managing complications. For personalized treatment plans and to consult the best surgical oncologists in Mumbai, seeking expert advice is essential.
Medically Reviewed By Dr. Amit Chakraborty
Updated on Sep 27, 2024
Surgical Management of Hypopharyngeal Cancer
Get an Enquiry

About Author
Dr Amit Chakraborty
Cancer Surgeon
Dr. Amit Chakraborty is a leading Head and Neck Surgical Oncologist in Mumbai with over 15 years of experience. A well-known cancer specialist for his expertise in treating oral, thyroid, buccal, laryngeal, hypopharyngeal, and parotid gland cancers through advanced surgical techniques and providing personalized care. Dr.Amit’s commitment to excellence has earned him recognition on both national and international platforms.
Read More