Oropharyngeal cancer is a serious but increasingly treatable disease that affects thousands of people each year. Understanding this condition from its early warning signs to modern treatment approaches can make a significant difference in outcomes. This comprehensive guide explores what oropharyngeal cancer is, its causes, symptoms, staging, treatment options, and survival rates based on the latest medical evidence.
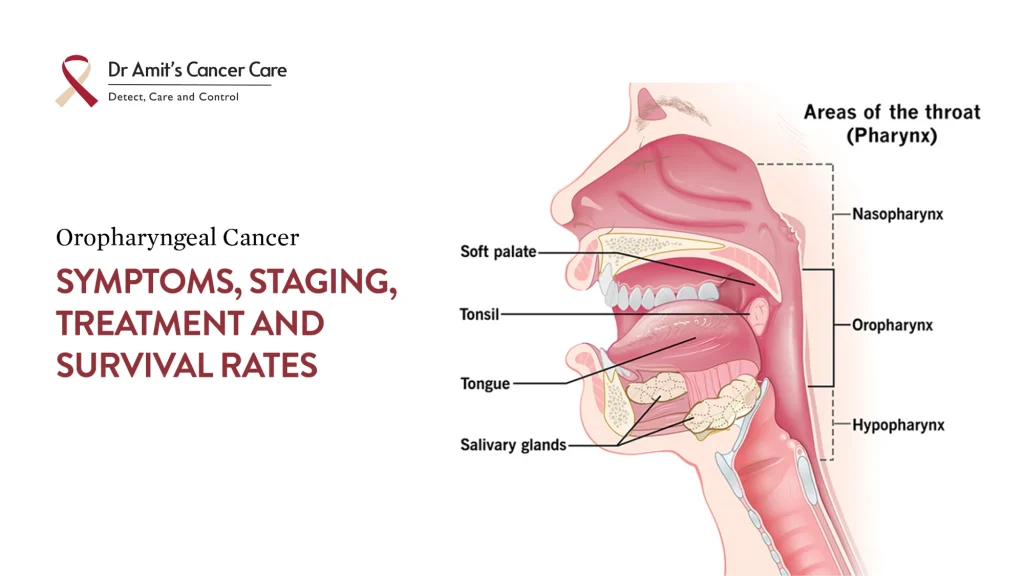
What Is Oropharyngeal Cancer?
Oropharyngeal cancer is a type of head and neck cancer that develops in the oropharynx, the middle section of the throat located behind the oral cavity. The oropharynx includes several anatomical structures:
- Base of the tongue (the posterior third of the tongue)
- Soft palate (the soft part of the roof of the mouth)
- Tonsils (both palatine tonsils)
- Pharyngeal walls (the side and back walls of the throat)
Most OPCs are squamous cell carcinomas (SCCs); i.e., cancer typically develops from squamous cells, which are the thin, flat cells lining the oropharynx.
A major recent evolution: OPC is now often divided into HPV-positive vs HPV-negative types, because their causes, prognosis, staging, and optimal treatments differ significantly. “HPV” refers to human papillomavirus, especially high-risk types like HPV-16.
What Causes Oropharyngeal Cancer?
OPC has several risk factors; some are modifiable. Here are the main ones:
| Cause / Risk Factor | Notes |
| HPV infection | A growing cause, particularly HPV-16. OPC that is HPV-positive tends to occur in people with fewer traditional risk exposures (e.g., less tobacco/alcohol). The virus’s oncoproteins (E6, E7) disrupt tumour suppressor pathways, increasing cancer risk. |
| Tobacco use (smoking, chewing) | Strongly associated with HPV-negative OPC, but also worsens outcomes even in HPV-positive cases. |
| Alcohol consumption | Especially chronic, heavy usage. Often acts synergistically with tobacco. |
| Oral sexual behaviour / sexual history | More sexual partners, earlier age at first exposure, etc., increase the risk of acquiring oral HPV infection. |
| Immune status | Immunocompromised individuals are more susceptible. Also, the ability to clear HPV infection is relevant. |
| Other possible risk factors | Poor oral hygiene, co‐infections, possibly dietary factors, betel nut chewing (in certain populations), and genetic susceptibility. |
Common Oropharyngeal Cancer Symptoms
Patients should be aware of the following warning signs:
Throat and Swallowing Symptoms:
- Persistent sore throat lasting more than two weeks that doesn’t respond to standard treatment
- Difficulty swallowing (dysphagia) or pain during swallowing (odynophagia)
- Sensation of a lump or foreign body in the throat
- Changes in voice quality or persistent hoarseness
Physical Manifestations:
- A palpable lump or mass in the neck (often the first noticeable sign)
- Unilateral ear pain (otalgia) without infection
- Unexplained weight loss
- White or red patches (leukoplakia or erythroplakia) in the mouth or throat
- Persistent bad breath (halitosis) not explained by dental issues
- Difficulty moving the tongue or jaw
Advanced Symptoms:
- Bleeding from the mouth or throat
- Breathing difficulties
- Persistent cough
- Numbness in the mouth or throat
- Obvious lumps/metastasis in the neck, possibly to distant sites
Important Note: Early-stage OPC may be completely asymptomatic or present with only minor throat irritation. This underscores the importance of regular dental and medical examinations, particularly for individuals with risk factors.
Staging of Oropharyngeal Cancer
Staging refers to assessing how far the cancer has spread: size of the primary tumour (T), involvement of lymph nodes (N), and distant metastasis (M). Accurate staging is crucial for prognosis and guiding treatment.
A major advance has been the 8th edition of the American Joint Committee on Cancer (AJCC)/UICC TNM staging system, which introduced separate staging criteria for HPV-associated (p16 positive) vs HPV-negative (p16 negative) OPC.
Here are the key points in staging:
- T (Tumour) categories: Describes the size and extent of the primary tumor
- T1: tumour ≤2 cm in greatest dimension
- T2: tumour >2 cm but ≤4 cm
- T3: tumour >4 cm or extension to specific structures
- T4: Very advanced local disease
- For HPV+ oropharyngeal cancer, T4a and T4b (in earlier staging) have been unified because differentiation didn’t correlate well with survival.
- N (Nodal) categories: Indicates lymph node involvement
- N0: No regional lymph node metastasis
- N1: Single ipsilateral node ≤3 cm
- N2: Multiple nodes or contralateral/bilateral nodes
- N3: Node >6 cm
And in HPV, it is categorised as:
- For example, in HPV+ OPC, ipsilateral lymph nodes ≤6 cm = cN1; contralateral or bilateral nodes ≤6 cm = cN2; nodes >6 cm = cN3.
- Pathologic N (pN) in HPV+ has categories based on the number of involved nodes, not laterality or size in some settings (e.g., pN1 = ≤4 nodes, pN2 = >4)
- Extranodal extension (ENE) plays a major role in staging for HPV disease.
- M (Metastasis): Presence of distant metastasis
- M0: No distant metastasis
- M1: Distant metastasis present
Any M1 is Stage IV in both HPV+ and HPV- types.
- Overall Stage Grouping: under the AJCC-8 staging, many HPV+ patients who would have formerly been “stage IV” under AJCC-7 are now stage I or II, reflecting their much better prognosis.
For HPV-Negative Oropharyngeal Cancer:
- Stage I: Small tumor, no lymph node involvement
- Stage II: Larger tumour or minimal lymph node involvement
- Stage III: Advanced local disease with significant nodal involvement
- Stage IVA/IVB: Very advanced local disease or extensive nodal disease
- Stage IVC: Distant metastases
For HPV-Positive Oropharyngeal Cancer: The staging system differs significantly, reflecting better outcomes. HPV-positive tumors are generally assigned lower stage designations for the same anatomical extent of disease compared to HPV-negative cancers.
The staging (clinical and pathological) is used to group patients roughly into Stages I through IV, with lower stages having smaller disease, less spread, and generally better prognosis.
Is Oropharyngeal Cancer Curable?
Yes, oropharyngeal cancer can be curable, especially when detected early, treated properly, and especially if it is HPV-positive. But “curable” depends on many factors: stage at diagnosis, patient’s general health, HPV status, location of the tumour, etc.
- HPV-positive OPC has a significantly better response to therapy (radiation, chemoradiation, surgery) and overall survival compared to HPV-negative OPC.
- Even among advanced stages, cure or long‐term control is possible, though with greater risk of recurrence, more aggressive treatment, and more side effects.
Thus, treatment goals may include cure (elimination of disease), and when that’s not feasible, palliation and prolongation of life with quality.
Treatment Options
Treatment depends on stage, HPV status, tumour location, patient health, and preferences. Here is a summary:
| Treatment Modality | Comments |
| Surgery | Removal of the primary tumour (transoral surgery, robotic surgery, or more invasive approaches depending on location) plus neck dissection if lymph nodes are involved.
More commonly used when a tumour is accessible and the patient is fit. |
| Radiation therapy (RT) | Often used alone or after surgery
(IMRT) It is standard to reduce damage to adjacent structures. |
| Chemoradiation (CRT) | Combined chemotherapy + RT for more advanced disease, to improve control and survival. |
| De-escalation approaches | In HPV-positive early stage disease, trials are exploring lower radiation dose / fewer chemotherapy cycles to reduce treatment toxicity while preserving high cure rates. For example, a phase 2 trial (2024) showed a reduced‐dose radiation + chemo approach in HPV+ throat cancer had 100% overall survival at a median of 2 years in the reduced treatment group. |
| Palliative treatments | For patients with distant metastases or not candidates for curative therapy, focus on quality of life, symptom relief (pain, swallowing, breathing). |
| Targeted Therapy |
|
| Immunotherapy |
|
Other important aspects:
Managing HPV status (though the vaccine works for prevention, not treatment once the disease is established)
Treatment by Stage
Early Stage (I-II):
- Surgery alone or radiation therapy alone are often sufficient
- Minimally invasive surgical approaches are preferred when possible
- Excellent cure rates with single-modality treatment
Locally Advanced Stage (III-IVB):
- Combined modality therapy typically required
- Surgery followed by radiation/chemoradiation, or
- Definitive chemoradiation (organ preservation approach)
- Treatment selection based on tumour location and patient factors
Metastatic Disease (IVC):
- Systemic chemotherapy and immunotherapy
- Radiation for symptom control
- Clinical trial consideration
Overall Survival Rates
- A study from a tertiary cancer care hospital in Kerala reported overall 5-year survival rates for oral cancer patients around 50-60%, with better survival in patients without lymph node involvement; the median disease-free survival was approximately 48 months. Node positivity was significantly associated with recurrence and worse outcomes. Early-stage oral cancers (Stage 1 and 2) in this setting had survival rates up to 80%, while advanced stages had lower survival (30-50%).
- Data from the Tata Memorial Hospital in Mumbai showed 5-year survival rates for localized oral cancers around 56% and 59% for loco-regional disease, comparable to international figures for similar stages.
- A comprehensive population-based cancer registry study under the Indian Council of Medical Research’s National Cancer Registry Programme (NCRP) analyzed oral cancer survival across multiple Indian regions, reporting a median 5-year survival of approximately 37%, with significant interstate variation ranging from about 20% to over 58%. This registry highlighted that squamous cell carcinoma cases had higher survival compared to non-SCC cases, and survival disparities correlated with differences in healthcare access and early detection.
- Another retrospective analysis at a tertiary center in central India found 5-year overall survival rates after treatment for oral squamous cell carcinoma of roughly 26%, with disease staging and nodal involvement strongly impacting outcomes.
Based on data from the Surveillance, Epidemiology, and End Results (SEER) database analysing cases diagnosed between 2015 and 2021, the five-year relative survival rate for oropharyngeal cancer is 57% across all stages combined.
However, survival varies significantly by the extent:
By Disease Extent:
- Localized disease (confined to the oropharynx): 62% five-year survival
- Regional disease (spread to nearby lymph nodes): 67% five-year survival
- Distant disease (metastasised to distant organs): 27% five-year survival
The somewhat counterintuitive finding that regional disease has slightly better survival than localised disease may reflect detection and treatment patterns. However, these rates are based on relatively small numbers of cases.
HPV Status and Prognosis
HPV status profoundly impacts survival outcomes:
HPV-Positive Oropharyngeal Cancer:
- Disease-free survival rates: 85-90% in five years
- Significantly reduced risk of death-approximately 60% lower compared to HPV-negative cases
- Better response to all treatment modalities
- Lower recurrence rates
- Most recurrences occur within the first year and at the primary site
HPV-Negative Oropharyngeal Cancer:
- Five-year survival rates: 25-40% in patients with traditional risk factors
- Higher rates of distant metastases
- Greater treatment resistance
Factors Affecting Curability
Several factors influence whether oropharyngeal cancer can be cured:
- Stage at diagnosis: Earlier detection dramatically improves outcomes
- HPV status: HPV-positive tumors have a superior prognosis
- Treatment response: Individual tumour biology affects therapy effectiveness
- Patient health: Overall fitness and absence of comorbidities
- Smoking status: Continued smoking worsens outcomes even during treatment
- tumour location: Some anatomical sites are more amenable to treatment
Staging & Survival: Putting It All Together
Because staging changed with the AJCC-8 system, comparing older studies is complicated. Key takeaways:
- Under AJCC-8, many HPV+ cancers are down-staged, meaning what used to be called Stage IV under AJCC-7 now might be Stage I or II. This reflects their much better prognosis.
- The presence of extranodal extension, the number of involved lymph nodes, and tumour size / local invasion remain important prognostic markers.
- Smoking history still matters: even in HPV+ OPC, heavy smoking worsens outcomes.
Conclusion
Oropharyngeal cancer is a serious disease, but one of the more treatable head and neck cancers, particularly when detected early and when HPV is involved. The rise of HPV-associated disease has changed the landscape: better prognosis, new staging systems, and more interest in reducing treatment intensity to spare side effects. Still, for the best outcomes, early diagnosis, personalized treatment, and attention to risk factors (tobacco, alcohol, and immune health) matter a lot.
Schedule a consultation with a head and neck cancer specialist or ENT doctor today. Regular check-ups, quitting tobacco, reducing alcohol use, and considering HPV vaccination are all proven steps that can lower your risk.
Your health is in your hands. Act early, act wisely.