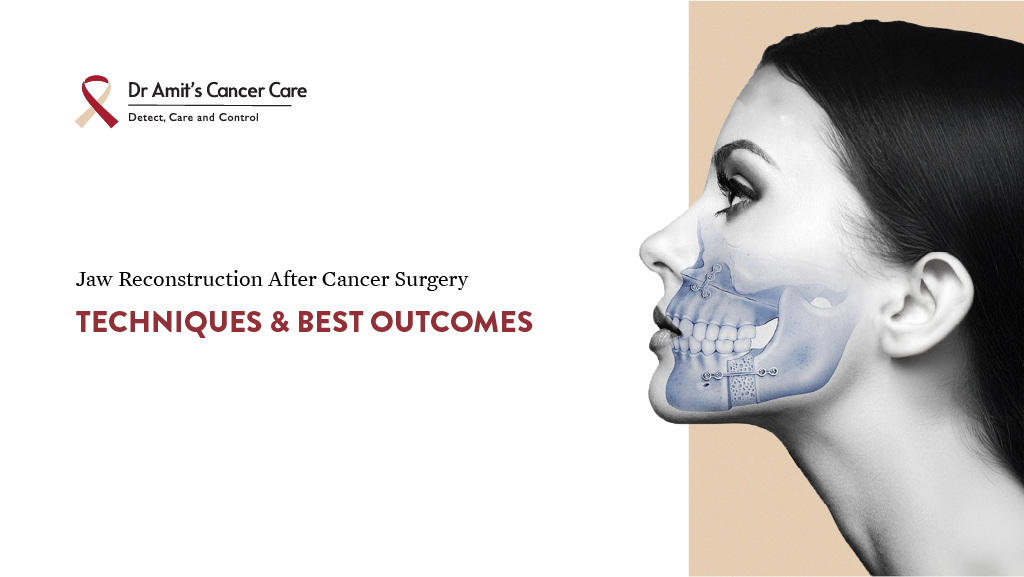
Facing jaw reconstruction surgery after cancer can feel overwhelming, but advances in surgical care have made it possible to restore both the function and appearance of the jaw with impressive success. Whether you’re considering jaw reconstruction surgery in Mumbai or elsewhere, understanding the process, available techniques, recovery, and long-term outcomes can help you make informed decisions.
This guide explains why jaw reconstruction is important after cancer, how the procedures work, what symptoms to watch for, and what to expect before, during, and after treatment.
Why Is Jaw Reconstruction Needed After Cancer?
When cancer affects the jawbone, especially the lower jaw (mandible), part of the bone may need to be surgically removed to ensure the complete elimination of cancerous tissue. This type of surgery, known as a mandibulectomy, is often critical for saving lives. However, it can also lead to serious challenges:
- Difficulty chewing and swallowing food
- Impaired speech due to loss of jaw support
- Visible changes in facial shape or symmetry
- Emotional or psychological stress from changes in appearance
That’s where jaw reconstruction surgery plays a vital role. It helps rebuild the jaw using your tissue or medical implants. The goal is not just to restore appearance, but also to bring back essential daily functions like eating, speaking, and smiling confidently.
Recognising the Early Symptoms of Jaw Cancer
Many patients seek help only after symptoms worsen. Recognising early warning signs can lead to faster diagnosis and better outcomes.
Here are common jawbone cancer symptoms to watch for:
- Swelling or a lump in the jaw or cheek area
- Persistent jaw pain that doesn’t improve with routine treatment
- Numbness in the lower lip or chin without dental cause
- Loose teeth or tooth displacement not related to gum disease
- Difficulty opening the mouth fully
- Non-healing sores or ulcers inside the mouth
- Jaw clicking accompanied by swelling or discomfort
While jaw clicking is most commonly associated with temporomandibular joint (TMJ) disorders, if it’s persistent and paired with other symptoms, it should be evaluated. Many people also overlook lower jaw cancer symptoms, which may seem like common dental issues but are persistent and gradually worsen.
If you notice any of these signs lasting more than two weeks, consult a dentist, oral surgeon, or ENT specialist for further evaluation.
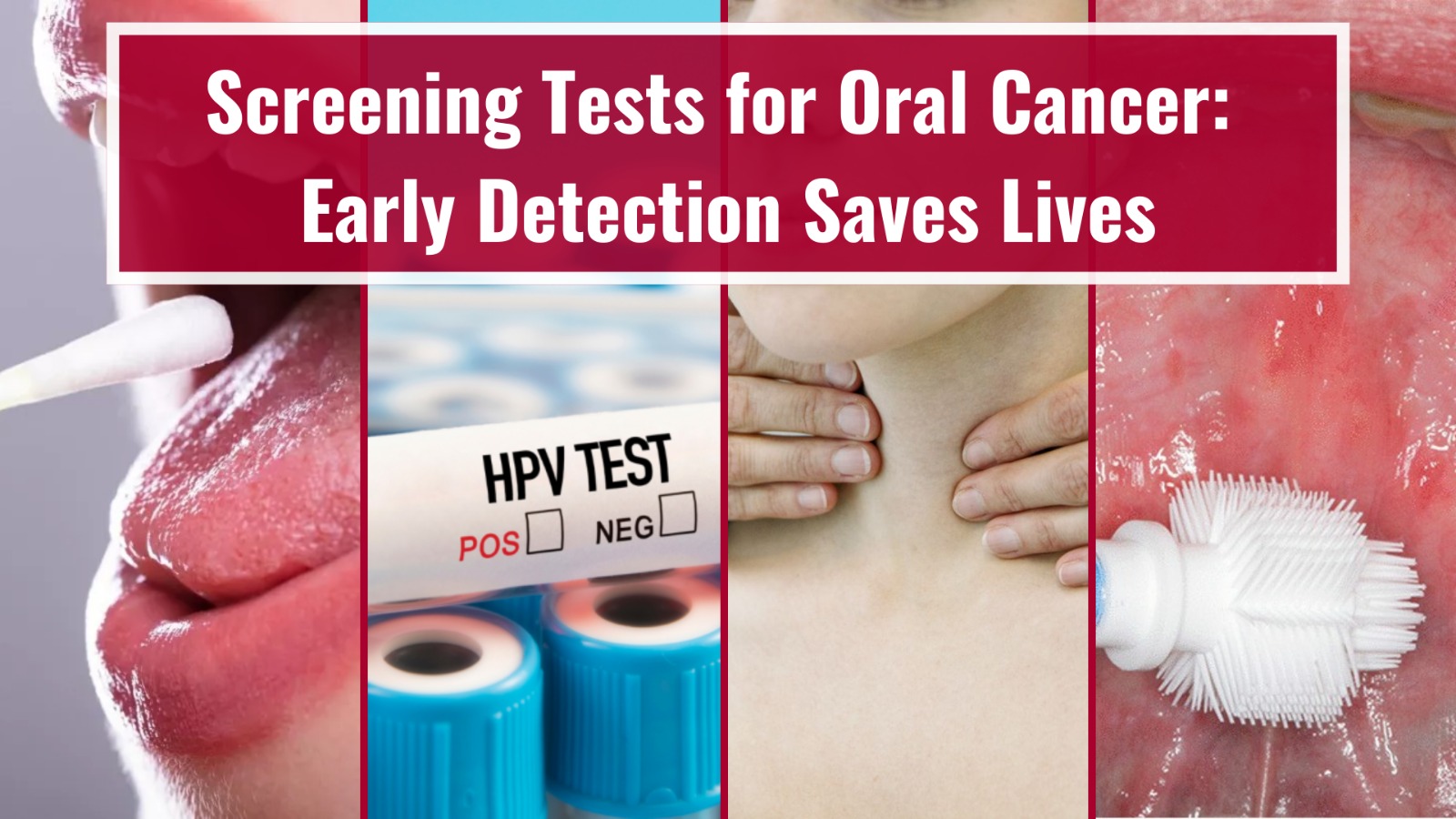
How is Jaw Cancer Diagnosed?
Diagnosing jawbone cancer involves a step-by-step process:
1. Clinical Examination
Your doctor will inspect the inside of your mouth and jaw area, feeling for lumps, swelling, or abnormalities.
2. Imaging Tests
CT scans, MRI, and sometimes PET scans are used to understand the extent of the tumour and its impact on surrounding tissues and bone.
3. Biopsy
A small tissue sample is taken from the suspicious area and examined under a microscope to confirm whether cancer is present.
These steps also help determine the stage of cancer and whether jawbone cancer surgery with reconstruction will be required.
Advanced Techniques in Jaw Reconstruction Surgery
Modern surgical advancements have revolutionised the way jaw reconstruction is performed. Here are the most commonly used and effective methods:
1. Fibula Free Flap Reconstruction
This is the most widely used and reliable technique. In this procedure:
- A section of bone is taken from the fibula (a bone in the lower leg), along with its surrounding tissue and blood vessels.
- The bone is reshaped to match the missing section of the jaw.
- Surgeons use microsurgery to connect the fibula’s blood vessels to those in the neck, ensuring the transplanted tissue remains healthy and integrates well.
The fibula is ideal because it provides enough bone for both structural support and possible dental implants in the future. Patients can usually walk normally after recovery, as the fibula is a non-weight-bearing bone.
2. Jaw-in-a-Day Surgery
Support from caregivers, dietitians, psychologists, and speech pathologists is important during this time to help with physical and emotional recovery.
3. 3D-Planned Surgery Using Virtual Models
Surgeons now use digital technology to plan the surgery in detail before entering the operating room.
- CT scans create a 3D model of your jaw.
- Surgeons use this to map out bone removal, reconstruction, and implant placement.
- Custom titanium plates and cutting guides improve precision and symmetry.
This reduces the time spent in surgery and helps deliver more predictable and aesthetic results.
Jaw Bone Cancer Survival Rates: What Does Research Say?
Survival rates for jawbone cancer depend on several factors:
- Stage and size of the tumour
- Whether cancer has spread to the lymph nodes or other areas
- Overall health and immune status of the patient
- Success of tumour removal and reconstruction
This approach is offered in some high-tech cancer centres. Here’s how it works:
- Cancer removal, jaw reconstruction, and placement of dental implants are done in one surgery.
- 3D planning and printing are used to create surgical guides for precise cuts and implant placement.
- This reduces the number of surgeries and speeds up both recovery and dental rehabilitation.
It’s ideal for select patients who are suitable for a single-stage surgery and want to restore appearance and function faster.
Who Should Consider Jaw Reconstruction?
Jaw reconstruction surgery is typically recommended in the following cases:
- When part of the jaw is removed due to cancer
- When the tumour affects both the bone and the surrounding tissues
- When there is a significant loss of function, such as difficulty chewing or speaking
- When facial appearance has changed due to cancer surgery
A team of specialists, including head and neck surgeons, oncologists, plastic surgeons, prosthodontists, and speech therapists, will collaborate to create a treatment plan tailored to your needs.
What Is the Recovery Process Like?
Recovery from jawbone cancer surgery with reconstruction takes time, but is manageable with the right care.
Here’s what most patients can expect:
- Hospital Stay: Usually 7 to 10 days after surgery.
- Diet: Starts with liquids, then shifts to soft foods. It may take weeks to return to a normal diet.
- Speech and Physical Therapy: Exercises help restore jaw movement, speech, and swallowing.
- Follow-ups: Regular checkups to monitor healing, check for cancer recurrence, and ensure graft success.
- Dental Implants: These may be placed immediately (in Jaw-in-a-Day cases) or after several months once healing is complete.
Research shows that patients who undergo reconstruction using vascularised fibula flaps in experienced cancer centres have high long-term survival rates. These patients often regain near-normal chewing and speech abilities. Early diagnosis and personalised treatment significantly improve both survival and quality of life.
Final Thoughts
Jaw reconstruction surgery after cancer is more than a cosmetic procedure. It is a key part of recovery that helps restore speech, eating, and self-confidence. Techniques like fibula free flap, Jaw-in-a-Day, and 3D planning make this possible with high precision and lasting results.
If you’re considering this treatment, especially jaw reconstruction surgery, choose a centre with experience in head and neck cancer care. A personalised plan can make a world of difference in your journey back to health.
At Dr. Amit Chakraborty’s clinic, patients receive personalised treatment plans designed to restore function and improve quality of life, guiding them through every stage of recovery.